The New Mediterranean Diet Cookbook community is unique!
Below you will find links to papers that we have contributed to the scientific literature, with emphasis on publications from that last few years.
Publications by Nicholas Norwitz, PhD
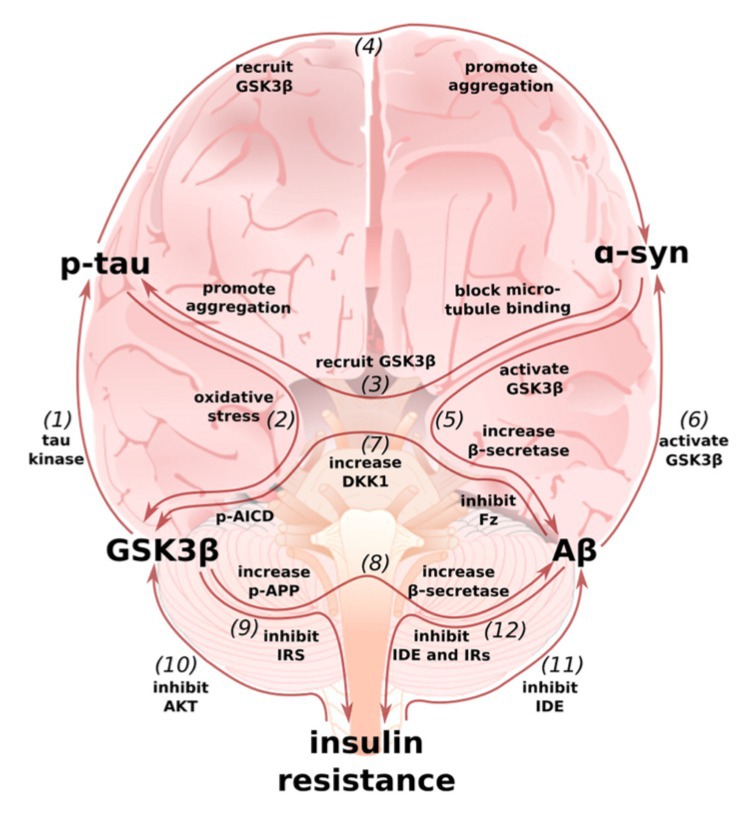
Alzheimer’s disease is ascending the list of the top ten causes of death and remains the only one without a treatment. This is, in large part, because Alzheimer’s disease begins in the brain decades before symptoms manifest. What we need to do is stop the disease before it starts in the brain, and this will require preventive nutrition!
The ApoE4 gene variant is the number one risk factor for Alzheimer’s disease, and most people who develop Alzheimer’s carry ApoE4 in their genome. By understanding how ApoE4 alters metabolism to increase Alzheimer’s risk, we can develop evidence-based precision nutrition approaches for preventing the disease. In this paper, we reviewed the top scientific literature from around the world on ApoE4 and, by understanding the biological mechanisms, developed a set of precision nutrition strategies to help prevent the disease.
The literature suggests, a Mediterranean-Ketogenic might be the best option for long-term brain health!
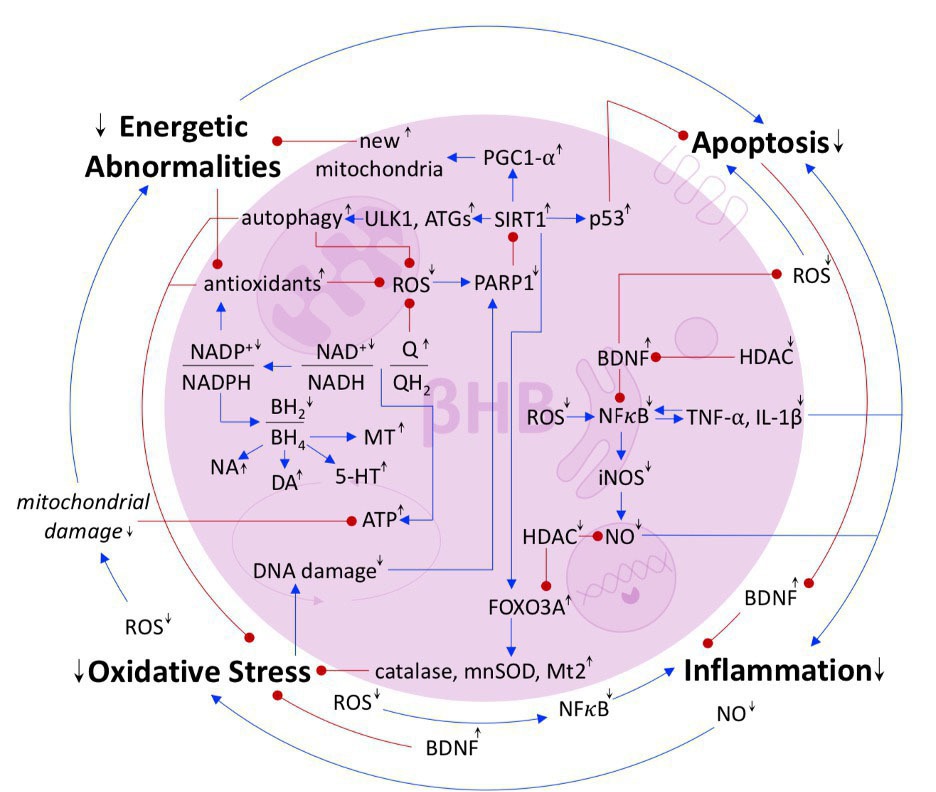
The notion that mental illnesses are just psychological problems is harmful in two ways. First, the belief that mental illnesses are purely a problem of the mind places a stigma on patients. Second, ignoring the metabolic nature of mental illnesses prevents health care professionals from providing complete care. This paper explains how mental illnesses are metabolic diseases and shows, through mechanisms and human evidence, that ketogenic diets can be successful in treating a variety of neurological diseases and mental illnesses.
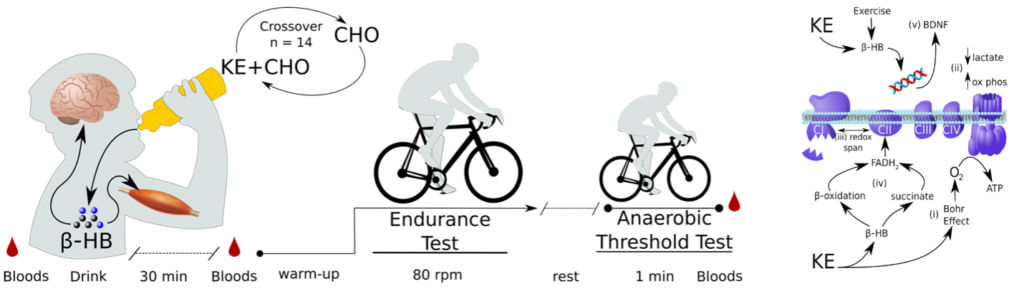
Parkinson’s disease is the second most prevalent neurodegenerative disease. Human trials suggest that ketogenic diets can help improve the symptoms of Parkinson’s disease. Separately, exercise is believed to help prevent and improve the progression of Parkinson’s disease. Therefore, we investigated whether the human ketone molecule, β-hydroxybutyrate, could itself improve exercise performance in people with Parkinson’s disease. In this randomized, placebo controlled, crossover trial, we show that ketones can improve exercise endurance capacity in Parkinson’s disease by an average of 24%!
In the general population, eating a modernized mixed-macronutrient diet, high LDL is associated with high levels of harmful small dense LDL particles, and also often associated low HDL and high triglycerides, two markers of metabolic syndrome. The constellation of high LDL, low HDL, and high triglycerides is called the “atherogenic lipid triad.” However, many people who go low-carb see an increase in their LDL while their HDL also increases and triglycerides decrease, which is a different pattern.
In addition, many patients also often observe improvements in waist circumference and visceral fat, small dense LDL, blood pressure, insulin resistance, and other risk factors for cardiovascular disease. Therefore, it’s not clear that an increase in LDL cholesterol, when it does occur in persons on a ketogenic diet, always constitutes an increase in risk. In this prospective case study, we followed an individual whole adopted a ketogenic diet with advanced lipid testing and observed that his LDL did, indeed, rise. However, this rise in LDL occurred without the “atherogenic lipid triad.” And, despite an overall tripling of his total LDL, his harmful small dense LDL actually decreased.
For more on this topic, please see:
Other recent peer-reviewed scientific papers authored by the team and book contributors
Nicholas Norwitz, PhD
Brianna Stubbs, PhD
Adrian Soto, MD PhD
Elena Gross, PhD
Chris Palmer, MD
Kieran Clarke, PhD
Read more here: Can Ketones Protect Against Alzheimer's Disease?
A selection of top reads by our friends and colleagues
In this long-term cohort study following 28,024 and over 50 clinical and metabolic markers for over two decades, insulin resistance was the strongest risk factor for coronary heart disease. LDL cholesterol was a weak risk factor and only small dense LDL, not big fluffy LDL that can go up on a ketogenic diet, was correlated with risk.
There are conflicting results on whether or not low-carb diets increase total energy expenditure (TEE) – the number of calories a person burns in a day. This may be because of differences in study duration. This meta-analysis of controlled studies revealed that this is the case. In short-term studies (<2.5 weeks), low-carb diets did not increase TEE; however, in the longer-term studies (>2.5 weeks), low-carb did increase TEE. This suggests both that low-carb diets can increase TEE and metabolic rate, consistent with other literature, and that short-term studies of fewer than about 3 weeks may not be fair in evaluating the pros and cons of low-carb diets. The body takes time to “fat-adapt.”
In this randomized controlled crossover study in individuals with metabolic syndrome, a low-carb diet reversed metabolic syndrome in 56% of participants in only 4 weeks. By comparison, a low-fat diet that included the same total calories and protein only reversed metabolic syndrome in 6% of people. These data suggest, even independent of caloric restriction, a low-carb diet has metabolic advantages over a low-fat diet for reversing metabolic syndrome.